SPOILER ALERT!
~ The amygdala communicates with many other brain structures including the brainstem.
~ The nuclei in the brainstem are involved in making us react if there is asphyxia or increased carbon dioxide (Co2) in the blood.
~ High Co2 in the blood (PC02) causes high pH in the blood, which can cause organ failure and even death.
~ Peripheral and central chemoreceptors alert the brainstem when there is a rise in PCo2.
~ High PC02 triggers hyperventilation to help clear Co2 build up.
~ With a healthy amygdala high PCo2 does not trigger panic attack and anxiety, but with damaged amygdala panic attack occurs.
~ Amygdala triggers transient episodes of apnea or "breathing pauses" in situations that could cause anxiety, such as at work, at social gathering, when reading a text or an email, etc…
"Breathing pauses" occur spontaneously as a response to an anxiety-provoking situation, but they don’t normally trigger panic attacks. However people with hypersensitivity to Co2 changes (such as panic disorder patients) tend to experience panic attacks when those pauses occur more frequently.
~ "Breathing pauses" are also observed in social anxiety, PTSD, and other phobias.
~ Because apprehensive anxiety develops in certain people, future episodes will be feared and avoidance behavior will appear.
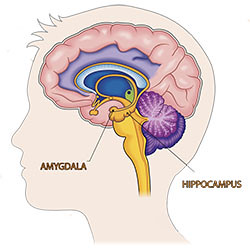
There is a large body of evidence showing that the amygdala plays a crucial role in the pathogenesis (the manner in which a disease develops) of anxiety and panic attacks; however the factors driving the chronicity of anxiety are still elusive to researchers. Interestingly, more recent research identifies a potential anxiogenic (i.e., causes anxiety) mechanism linking the amygdala and carbon dioxide (Co2) sensors .
The Role of the Amygdala in Respiration
The amygdala is the most connected structure in the brain with its thirteen sub-nuclei, each with its own pattern of connectivity. The most noteworthy connectivity involves that with the nuclei in the brainstem, which is a structure responsible for regulating systems that are under involuntary control.
The brainstem nuclei are critically involved in autonomic regulation including life-supporting functions such as heartbeat and breathing. Particularly relevant is their role in inducing arousal following asphyxia and increased Co2 in the blood.
Peripheral and central chemoreceptors projecting into the brainstem are responsible for detecting changes in Co2 in the blood (called partial pressure of Co2 or PCo2 for short) and pH levels (normal blood pH is between 7.95 and 7.45. Small shifts from this range trigger compensatory changes in respiration, since changes in blood acidity can potentially lead to organ failure and death).
As PCo2 rises and pH becomes more acidic, respiratory chemoreceptors trigger a suffocation alarm (i.e., similar to air hunger) resulting in the initiation of hyperventilation (i.e, increased respiration to get rid of the accumulated Co2), and the induction of fear, anxiety and panic in certain cases.
Thus, it is through its network that the amygdala exerts an influence on respiratory regulation and in the generation of fear and anxiety.
Amygdala Activation Inhibits Panic
Clues about the role of the amygdala in panic and anxiety come from studies of patients with bilateral amygdalar lesions (i.e., damage to both amygdalae). Specifically, it was found that while those patients are unable to feel fear or panic when exposed to fear-inducing external stimuli (e.g., a snake, horror movies, haunted house, and other traumatic life events), they experience intense fear, even panic attacks, when inhaling a mixture of 35% Co2 (typically the air we breathe contains only ~0.4%).
This episode of panic is akin to what individuals with panic disorder experience, including air hunger and hyperventilation. By contrast, healthy participants exposed to the same mixture do not panic, but they do hyperventilate.
Further investigations led to the discovery of the inhibitory role of the amygdala in respiration. More particularly, it has been proposed that when stimulated the amygdala triggers transient episodes of apnea (stop breathing) through inhibitory action on the brainstem, which then results in transient spikes in Co2.
There is a certain threshold beyond which activation of the amygdala induces transient apnea and once its activation has subsided, its inhibitory action on the brainstem is lifted and breathing resumes. As breathing resumes, the person could feel anxiety and even panic as a result of the build-up of Co2. Therefore, activation of the amygdala prevents the initiation of a panic attack.
Naturally Occurring Breathing Pauses
It follows then that individuals with hyperactive amygdala are at a high risk for experiencing panic attacks following those transient apneic episodes, particularly if they have a high sensitivity to Co2. This would be consistent with reports indicating that patients with panic disorder consistently experience a panic attack when inhaling a mixture of 35% Co2.
The ability of the amygdala to stop breathing is thought to have evolutionary roots. Indeed, it could be a manifestation of the freezing response observed in both humans and animals when exposed to danger. For example, in the wild a prey would stop breathing momentarily to avoid detection by a predator.
Similarly, instances that could trigger these states of apnea abound in everyday life during anxiety-inducing situations such as at work, at a social gathering, when opening an email, or even when engaging in social media. These situations potentially trigger ‘breathing pauses” due to their anxiogenic (cause anxiety) context.
For example, studies using ambulatory monitoring (i.e., portable monitors that track specific physiological markers like blood pressure, oxygen saturation, etc…) reveal that healthy individuals experience increased patterns of sustained “breathing pauses” in social gatherings compared to when they are alone. These pauses are also associated with high blood pressure.
Furthermore, another study found that panic disorder (PD) patients also experience “breathing pauses” lasting anywhere between 20 and 60 seconds with the longest ones followed by panic attacks. These breathing irregularities in PD manifest themselves as hyperventilation and constant sighing, which are compensatory behaviors designed to help clear the Co2 build-up.
Lastly, due to the nature of anxiety, individuals who are hypersensitive to Co2 changes are more likely to develop apprehensive anxiety and thus fear future episodes. They are also most likely to engage in avoidance behavior by associating a place or an event with their last panic attack, resulting in their compulsive avoidance of said place or event. This turn of event likely contributes to the maintenance of anxiety and even its worsening.
Reference:
Feinstein JS, Gould D, Khalsa SS. Amygdala-driven apnea and the chemoreceptive origin of anxiety. Biol Psychol. 2022 Apr;170:108305. doi: 10.1016/j.biopsycho.2022.108305. Epub 2022 Mar 7. PMID: 35271957.